
What is Lipedema?
February 26, 2023

By Dr. Steff
Surgeon. Humbled to serve.
Background
Lipedema is an under-diagnosed, loose connective tissue disease that many people are not aware. Seen in 11% of women worldwide (this number is variable based on the source), there is an increased build-up of fat in the lower part of the body that includes the abdomen, buttocks, hips, and legs as well as the arms, at times.1,2,5,8 It typically affects women, and there can be a genetic component to the disease.4 Inflammation is one of the leading causes of fat accumulation.2 Weight loss programs and even weight loss surgery can be ineffective.
It typically affects women, and there can be a genetic component to the disease.
What causes Lipedema?
There is an increased amount of fat that accumulates under the skin in the lower abdomen, legs, hips, and arms. A biochemical process in the soft tissue, which include fat and other cells under the skin, leads to swelling from water collection as well as increased fat accumulation.2 Most of these changes occur during times of natural body changes such as puberty, menopause, stress, trauma, and childbirth to name a few.2
Biochemistry
Certain molecules called proteoglycans whose quantities are increased in the soft tissue layer tend to bind to water molecules.2,3 As more water gets bound and also flows naturally into this layer, fluid builds up and prevents cells in the fatty layer from getting enough oxygen. This lack of oxygen leads to inflammation and fibrosis.2 There is also an increase in salt levels found in the skin of Lipedema patients.2
Aldo-Keto Reductase 1C1 is linked to Lipedema
Genes
Genetic studies are ongoing. There appears to be one gene called Aldo-Keto Reductase 1C1 that is linked to Lipedema.4 Due to this defective gene, there is increased fat build up from a slower chemical reduction of the hormone, progesterone, to hydroxy progesterone, which should prevent the fat from accumulating.4
Do I have Lipedema?
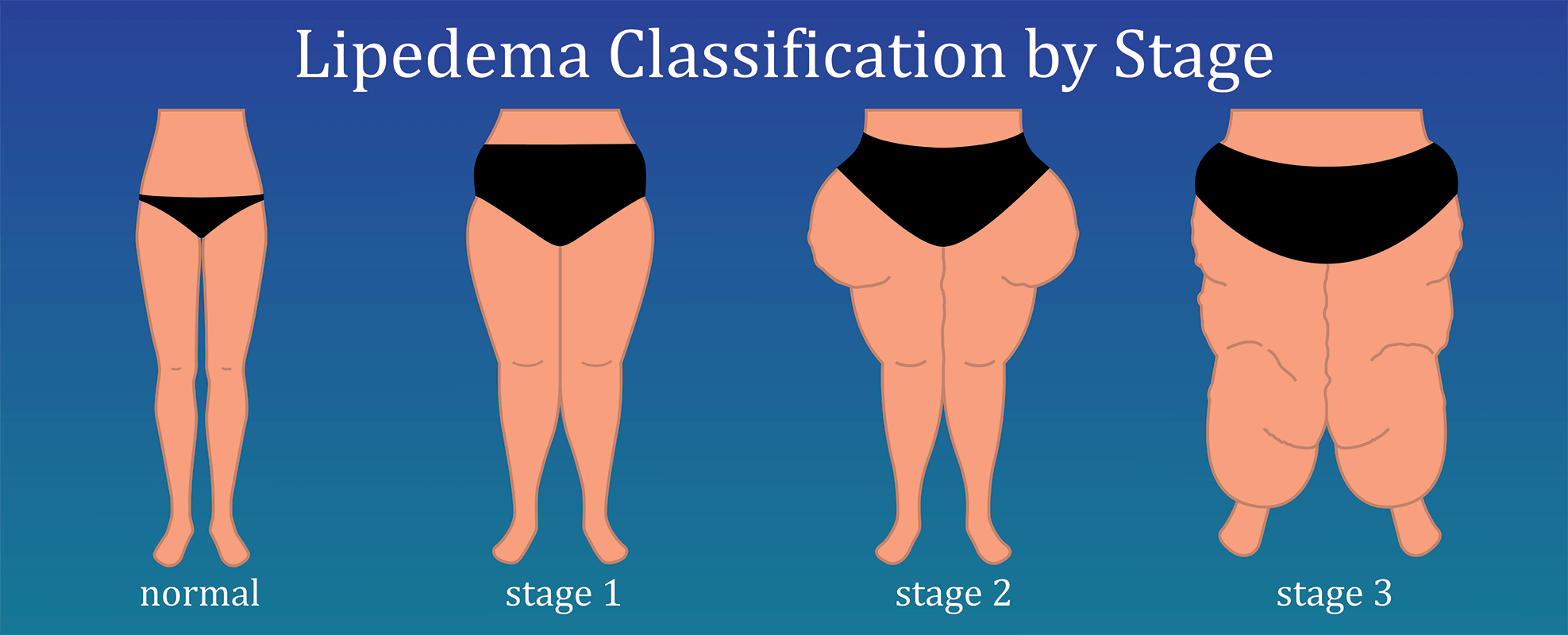
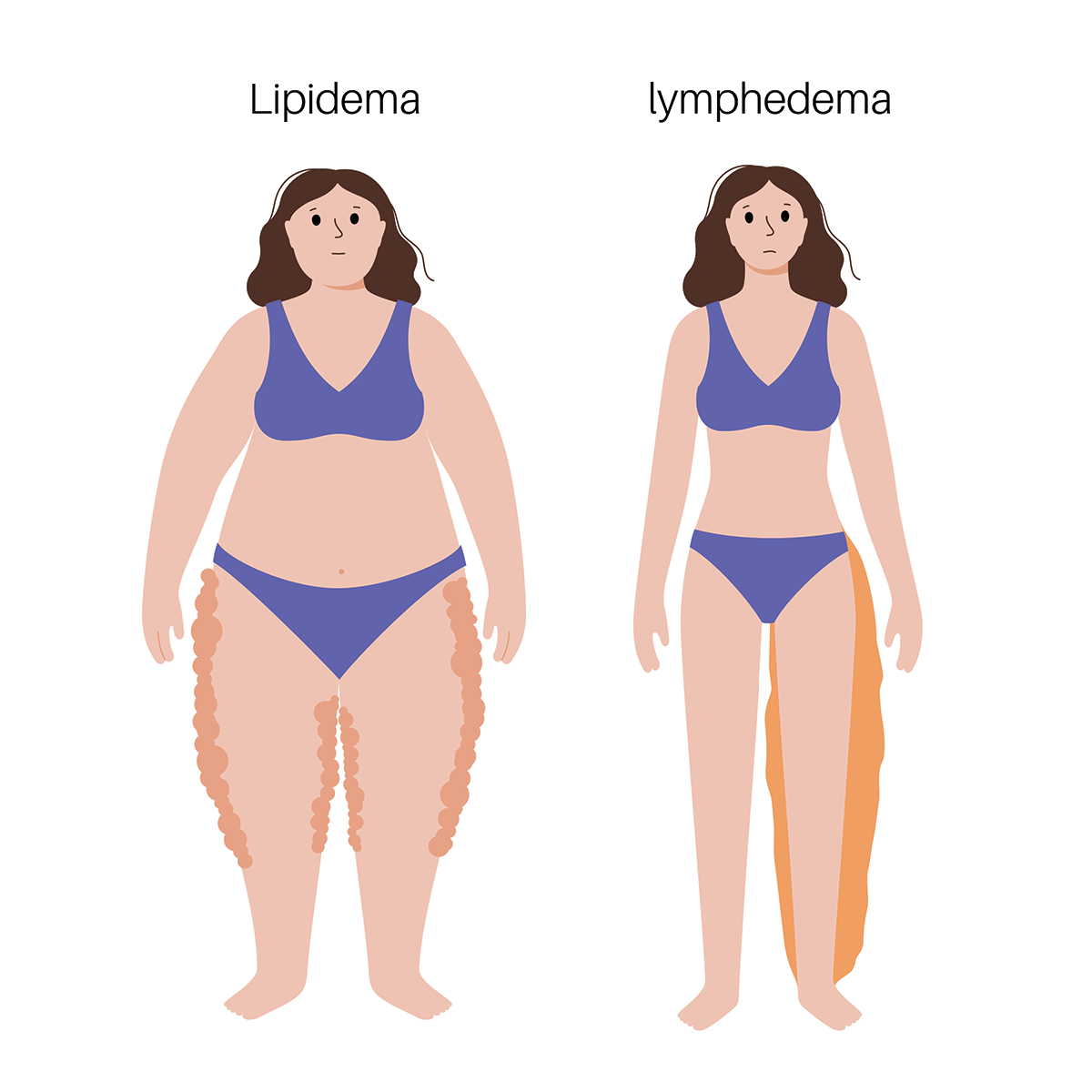
Diagnosis is based on your physical exam, history, and medical conditions. On the physical exam, patients have a certain appearance that can include enlargement of the girth of the lower abdomen, hips, and legs. There could be ankle cuffing, overhanging soft tissue above the elbows, ankle stance change, flat feet, sparing of the hands and feet from fat deposition, and spine changes that are present.2,5 These physical attributes and symptomatic characteristics are observed in the staging of Lipedema.5
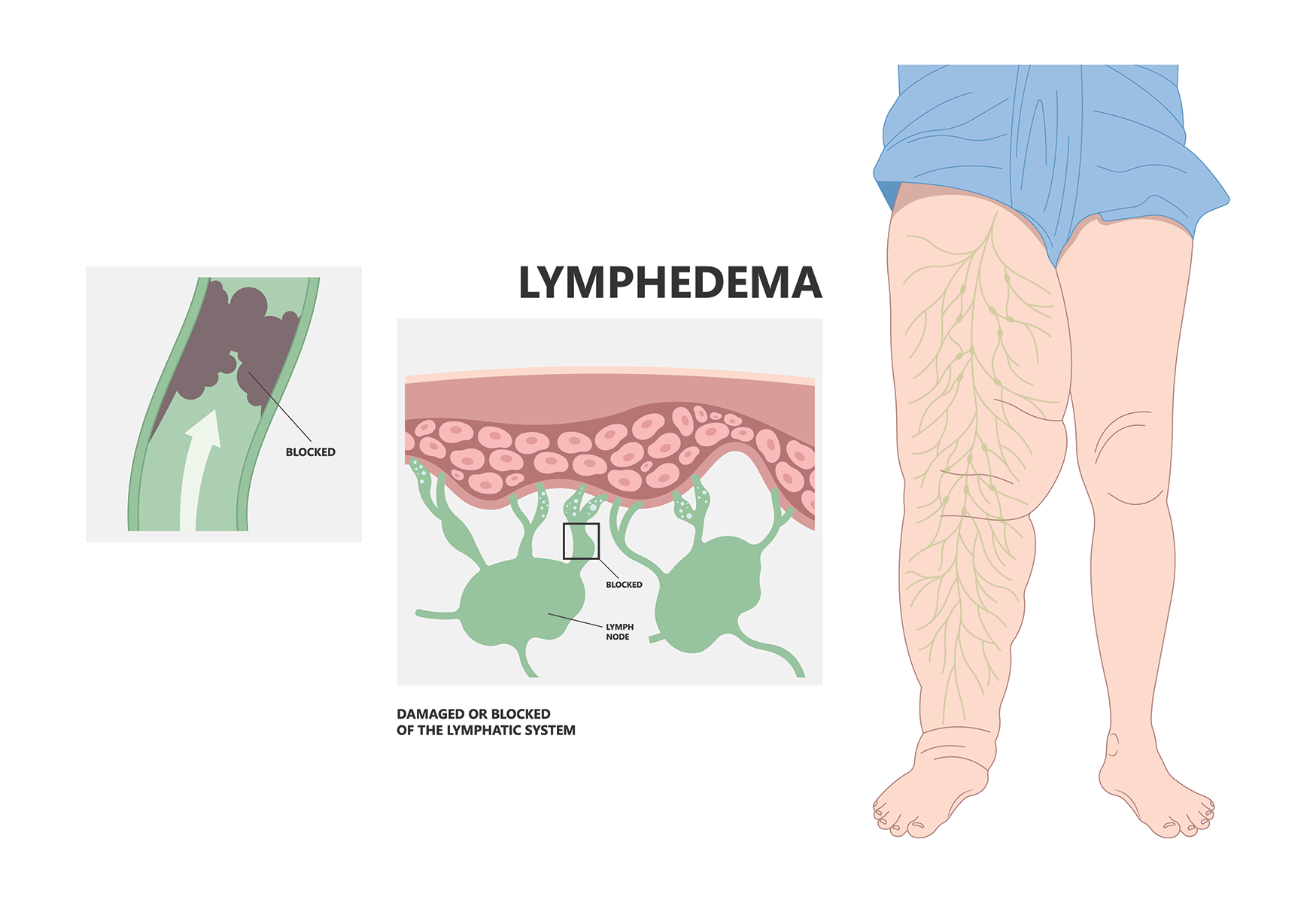
As the disease worsens, patients may experience lymphedema (i.e., enlarged lymph vessels and/or malfunction of lymph system), venous hypertension (i.e., valves in leg veins malfunctioning), non-lipedema obesity, easy bruising, skin and soft tissue loss of elastic properties, painful soft tissue, and hyper-flexible joints.2,6,7,11 Of note, not all symptoms may be present.
Additional findings in Lipedema patients can include low thyroid and vitamin D levels.2,8,9,10
No current lab test exists to confirm Lipedema, but there may be in the future.
What are some health issues commonly seen amongst patients with Lipedema?
- As one's weight increases, arthritis can develop in the joints of the legs as well changes in gait and posture that can lead to pain.2,8,12
- Vitamin D deficiency is noted as BMI (body mass index) increases.2,10 Vitamin D is important for bone health and prevention/management of osteoporosis , which is a disease that causes degeneration of bone. If one's bones degenerate, they are more likely to fracture.
- Hypothyroidism from low thyroid hormone levels can cause one to be tired, depressed, constipated, gain additional weight, and develop muscle aches to name a few symptoms.2,8,9
- Sleep disorders such as sleep apnea may be present.2,8
- Mental health conditions such as eating disorders and depression can be prevalent.2,10, 12
This is a brief list that does not mention all symptoms that can be associated with Lipedema.
What is the treatment for Lipedema?
Medical management includes looking at ones existing medication list and avoiding medicine that predisposes one to build up fat. There are some studies to indicate that Diosmin can improve the oxidative state and lead to relief of certain symptoms.2 Speak to your doctor about starting treatment for other symptoms that can develop due to this disease.
Surgical management with fat reduction procedures such as liposuction is also helpful.2,11 Gastric bypass surgery may not be as effective.
Venous disease and lymphedema should be addressed if present. Venous disease is diagnosed with clinical assessment and imaging that includes an ultrasound. Lymphatic disease is diagnosed with clinical assessment and diagnostic tools such as lymphoscintigraphy. Compression stockings of a certain strength (recommended by a medical provider) and venous and lymph procedures may be needed for symptoms relief. Peripheral arterial disease (i.e., blockages of leg arteries) can also lead to leg pain, so seek a medical provider's opinion.
Patients should start treatment early, esp. to control symptoms of lipedema, before comorbidities get worse (or prevent these health issues from developing).
Buck DW 2nd, Herbst KL. Lipedema: A Relatively Common Disease with Extremely Common Misconceptions. Plast Reconstr Surg Glob Open. 2016 Sep 28;4(9):e1043. doi: 10.1097/GOX.0000000000001043. PMID: 27757353; PMCID: PMC5055019. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5055019/)
Herbst KL, Kahn LA, Iker E, et al. Standard of care for lipedema in the United States. Phlebology. 2021;36(10):779-796. doi:10.1177/02683555211015887. (https://journals.sagepub.com/doi/full/10.1177/02683555211015887?rfr_dat=cr_pub++0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org)
Allen M, Schwartz M, Herbst KL. Interstitial Fluid in Lipedema and Control Skin. Womens Health Rep (New Rochelle). 2020 Oct 14;1(1):480-487. doi: 10.1089/whr.2020.0086. PMID: 33786515; PMCID: PMC7784769. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7784769/).
Michelini S, Chiurazzi P, Marino V, Dell'Orco D, Manara E, Baglivo M, Fiorentino A, Maltese PE, Pinelli M, Herbst KL, Dautaj A, Bertelli M. Aldo-Keto Reductase 1C1 (AKR1C1) as the First Mutated Gene in a Family with Nonsyndromic Primary Lipedema. Int J Mol Sci. 2020 Aug 29;21(17):6264. doi: 10.3390/ijms21176264. PMID: 32872468; PMCID: PMC7503355. (https://www.mdpi.com/1422-0067/21/17/6264)
Kruppa P, Georgiou I, Biermann N, Prantl L, Klein-Weigel P, Ghods M. Lipedema-Pathogenesis, Diagnosis, and Treatment Options. Dtsch Arztebl Int. 2020 Jun 1;117(22-23):396-403. doi: 10.3238/arztebl.2020.0396. PMID: 32762835; PMCID: PMC7465366. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7465366/)
Rasmussen JC, Aldrich MB, Fife CE, Herbst KL, Sevick-Muraca EM. Lymphatic function and anatomy in early stages of lipedema. Obesity (Silver Spring). 2022 Jul;30(7):1391-1400. doi: 10.1002/oby.23458. Epub 2022 Jun 15. PMID: 35707862; PMCID: PMC9542082. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9542082/pdf/OBY-30-1391.pdf)
Chakraborty A, Crescenzi R, Usman TA, Reyna AJ, Garza ME, Al-Ghadban S, Herbst KL, Donahue PMC, Rutkowski JM. Indications of Peripheral Pain, Dermal Hypersensitivity, and Neurogenic Inflammation in Patients with Lipedema. Int J Mol Sci. 2022 Sep 7;23(18):10313. doi: 10.3390/ijms231810313. PMID: 36142221; PMCID: PMC9499469. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9499469/pdf/ijms-23-10313.pdf)
Herbst K, Mirkovskaya L, Bharhagava A, et al. Lipedema fat and signs and symptoms of illness, increase with advancing stage. Arch Med 2015; 7: 1–8. (https://www.lipoedema.co.uk/wp-content/uploads/2016/01/lipedema-fat-and-signs-and-symptoms-of-illness-increase-with-advancing-stage.pdf)
Bauer AT, von Lukowicz D, Lossagk K, Aitzetmueller M, Moog P, Cerny M, Erne H, Schmauss D, Duscher D, Machens HG. New Insights on Lipedema: The Enigmatic Disease of the Peripheral Fat. Plast Reconstr Surg. 2019 Dec;144(6):1475-1484. doi: 10.1097/PRS.0000000000006280. PMID: 31764671.
Cannataro R, Cione E. Nutritional Supplements and Lipedema: Scientific and Rational Use. Nutraceuticals. 2022; 2(4):270-277. https://doi.org/10.3390/nutraceuticals2040020
Anne Warren Peled & Elisabeth A Kappos (2016) Lipedema: diagnostic and management challenges, International Journal of Women's Health, 8:, 389-395, DOI: 10.2147/IJWH.S106227. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4986968/pdf/ijwh-8-389.pdf)
Vyas A, Adnan G. Lipedema. [Updated 2022 Sep 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK573066/